Strokes can happen to any adult, at any time. People of all ages should be prepared to identify a stroke happening to yourself, or someone you love.
Strokes are when the brain becomes damaged due to a lack of blood supply. Knowing the signs of a stroke can help make the biggest difference in getting care and recovering.
There’s more than one type of stroke. In fact, there are five stroke types: ischemic, hemorrhagic, transient ischemic attacks (TIA), cryptogenic, and brain stem strokes.
(iz-keem-ic) This kind accounts for 87% of all strokes. Ischemic strokes are caused by blood clots:
This type of stroke occurs when a weakened blood vessel bleeds.
These strokes include a temporary blockage of a blood vessel that usually lasts less than 5 minutes. Symptoms may last minutes to 24 hours, and are not permanent. Take a TIA type stroke as a warning sign that another stroke may be coming. Seek medical help as soon as you can.
Strokes with unknown causes are called Cryptogenic.
This is a stroke to the brain stem. It often includes complex symptoms, and accounts for about 10-15% of all strokes.
Stroke risk is more lifestyle-dependent than any other factor. The brain requires blood; when blood flow is restricted, you may suffer a stroke. One example is a Carotid Artery Dissection (CAD) or Vertebral Artery Dissection (VAD)—an injury to either of these arteries can cause an ischemic stroke.
While strokes are less likely in young people, blunt trauma (from sports or a car accident) and resulting arterial dissection can cause a stroke. However, strokes are typically a result of a life-long accumulation of eating foods with little nutritional value, not staying active, and simply getting older, which can lead to diabetes, hypertension and weight gain.
Our body works similarly to a plumbing system. Over time, things build up. A clog could either prevent the flow entirely, or it could break free and make its way to somewhere worse.
There are plenty of stroke risk factors—some avoidable, and some not:
High Blood Pressure – People with blood pressure over 120/80 mmHg are at higher risk for stroke. Nearly half of all Americans have high blood pressure.
Diabetes – Patients with diabetes are twice as likely to have a stroke than those without Diabetes.
Any of the following will put you at greater risk for stroke: Atrial Fibrillation, coronary heart disease, heart valve disease, or carotid artery disease. When the heart needs to regularly work harder it will be less effective in pumping blood to where it needs to go (the brain).
Low Density Lipoprotein (LDL) is commonly referred to as the “bad” cholesterol. High cholesterol can result in narrowing of the arteries and increase risk for clots.
Smoking is a huge contributor of cardiovascular disease. Smoking can also raise the triglyceride (fat) level in your blood, lower your “good” cholesterol (HDL) and make your blood sticky and more likely to clot—which can lead to stroke.
Brain Aneurysms and AVMs – Arteriovenous Malformations (AVMs) are when blood passes quickly from an artery to a vein in a tangled connection—if an AVM ruptures in the brain, it can cause a stroke. When a brain aneurysm ruptures (also called a vasospasm) blood vessels may narrow or contract, restricting flow to the brain, causing an ischemic stroke.
Women are more likely (after age 25) to have strokes than men. Some related risks occur with pregnancy, such as pregnancy-induced high-blood pressure or gestational diabetes, while certain birth control medicines and post-menopausal hormone therapy can also put women at risk for stroke.
African Americans, American Indians, Alaska Native Americans, and Hispanic Americans are more likely than white Americans to have a stroke.
This risk factor is closely linked to hereditary predisposition to other risk factors, such as high blood pressure. It’s also common to have stressors and lifestyle choices that are similar to family members who may have suffered a stroke. However, some genetic disorders, such as sickle cell disease, can cause stroke. Pay attention to the illnesses and conditions of your family members.
The two main reasons patients come to see a chiropractor are neck pain and headaches, but these can also indicate artery dissection. If we suspect this is happening, we will send you to the emergency room immediately.
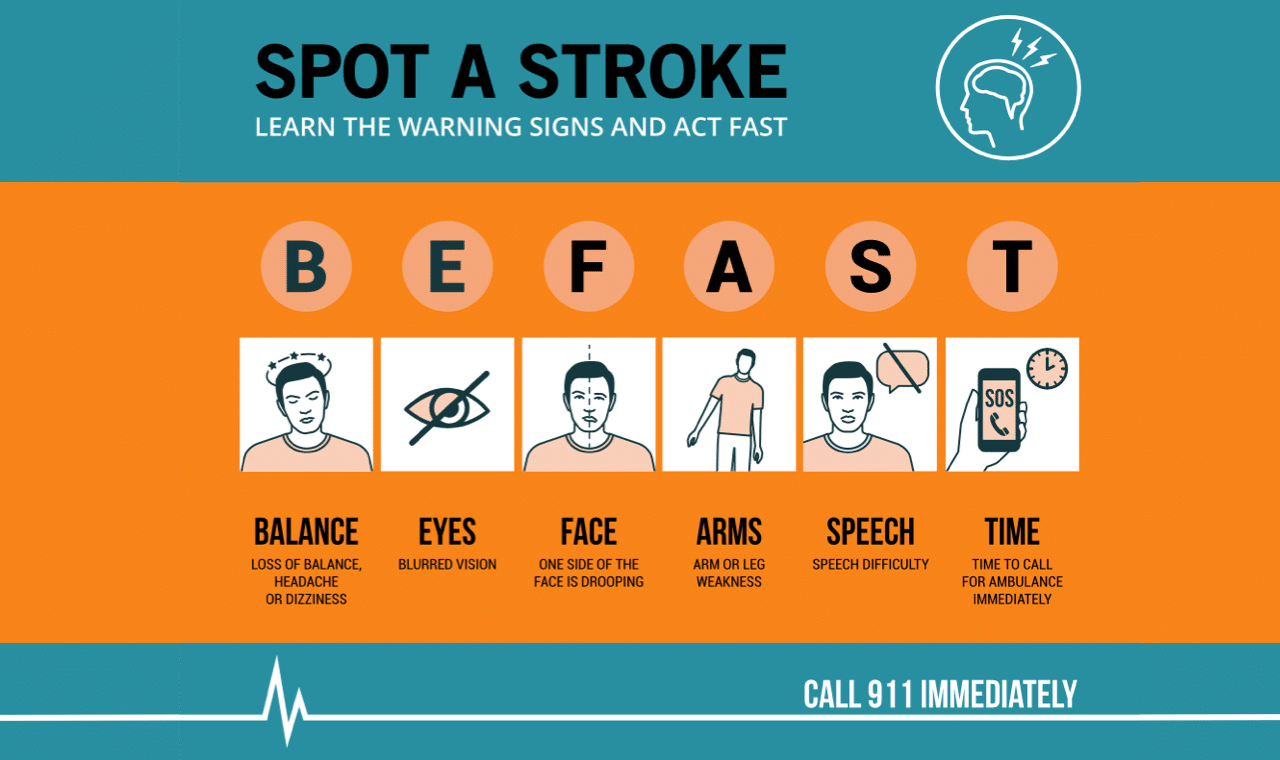
Look for the classic signs of stroke, and think BEFAST:
B – Balance, dizziness, headache
E – Eyes or blurry vision
F – Facial drooping
A – Arm weakness
S – Slurred speech
T – Time to call 911
Pay attention to a sudden onset of any, some, or all of the following signs of a stroke as well:
Time is not on your side with stroke treatment. Quickly seek help, as the sooner treatment is rendered, the better the outcomes may be. At the hospital, treatment for stroke may include medication to break up clots, blood thinners, stents for ischemic strokes, and medication/surgery for a hemorrhagic stroke.
Recovery from a stroke depends on the severity of the symptoms, but recovery often includes physical therapy, occupational therapy, speech therapy, and neurorehabilitation.
In April, my father suffered a stroke.
My dad is a healthy, active 70-year-old who competitively water skis, plays pickleball every day, and competes in long distance off-road races, among other hobbies. He eats a pretty healthy diet, doesn’t smoke, has a Coors Light or two each day, and his only relative health symptom is mildly high cholesterol.
He was water skiing as he does most Sundays; he was pulling out the wake, when he suddenly fell. His initial complaint was a tingling left arm and having a hard time getting back up when he tried to continue skiing. His symptoms progressed over the evening to include whole left arm numbness, difficulty walking on his left leg and difficulty coordinating movement with his left arm and left face numbness. He finally went to the ER the next morning. He did not have the classic stroke signs, but after a brain MRI, it was confirmed that he had had a right basal ganglia ischemic stroke. In hindsight, he believes that he fell skiing because his left arm lost control, which was when he probably had the stroke. He may have residual motor and sensory deficits, but he is lucky as far as strokes go.
When we chatted more about this water skiing numbness and tingling, he determined he may have had a TIA stroke last August. He is doing well so far, even though he didn’t go in right away.
Learn from my father—don’t ignore things, and don’t wait too long to get care. Sometimes you’ll get a warning sign, but sometimes you won’t. If you catch it early on, you may receive blood thinners to prevent clot formation and any additional strokes. Your treatment and recovery varies widely depending on when you seek care.
Go in before it becomes serious, and always think BEFAST.
Copyright @2025 Element Chiropractic — 875 SW Rimrock Way Suite 103, Redmond, OR 97756